The long-held view that carbohydrate-rich foods are protective against heart disease, or at least benign, turns out to be wrong. Carbohydrate recommendations are too high but which carbohydrate-rich foods should be recommended in a healthy diet and which foods should be culled?
One of the most important findings from nutrition research in recent years was that carbohydrate confers similar risk for coronary heart disease to saturated fat. This turned 20 years of dietary advice on its head as it meant that the long-recommended low fat diet was not protective against heart disease. It followed that carbohydrate recommendations were too high and if lower intakes of carbohydrate were to be recommended, it would make sense to preference ‘good’ carbohydrate.
But what is good carbohydrate? Ask this question to a room full of nutritionists and the argument will go on for hours. Thirty years ago starch was considered good and sugars were bad, based on the assumption that starch was digested more slowly and raised blood glucose levels more gradually than sugars. However, studies of glycaemic index showed this assumption to be wrong. So should nutritionists forget about sugar and start recommending low GI foods? There are also arguments over whether ‘wholegrain’ or dietary fibre is the better measure of a good cereal food. In the United States, nutrition authorities have adopted nutrient density as an over-arching principle of their latest dietary guidelines. It would certainly make sense to favour nutrient-rich carbohydrate foods if total carbohydrate intake (or calories) was to be limited. So there are lots of options and opinions but no consensus on what represents good and bad carbohydrate.
Against this swirling background Professor Manny Noakes from CSIRO and I recently published a new model for assessing the nutritional quality of carbohydrate-rich foods.
Assessing nutritional quality
The new model has now been published in the journal Nutrition and Dietetics so it won’t be reviewed in detail here. Instead I’ll highlight some of the more challenging findings.
The model assesses the nutritional quality of carbohydrate-rich foods based on their nutrient density and glycaemic index. Nutrient density was chosen as it reflects the fundamental nutritional role of food – to provide the body with essential nutrients. Glycaemic index was included as it captures how the body responds to the carbohydrate per se. Both measures were thought to be objective and therefore applicable to all carbohydrate-rich foods and drinks. Subjective measures of nutritional quality were avoided e.g. whether foods were natural, fresh, traditionally considered healthy, processed or ‘junk’. The challenge was to demonstrate the nutritional quality of foods.
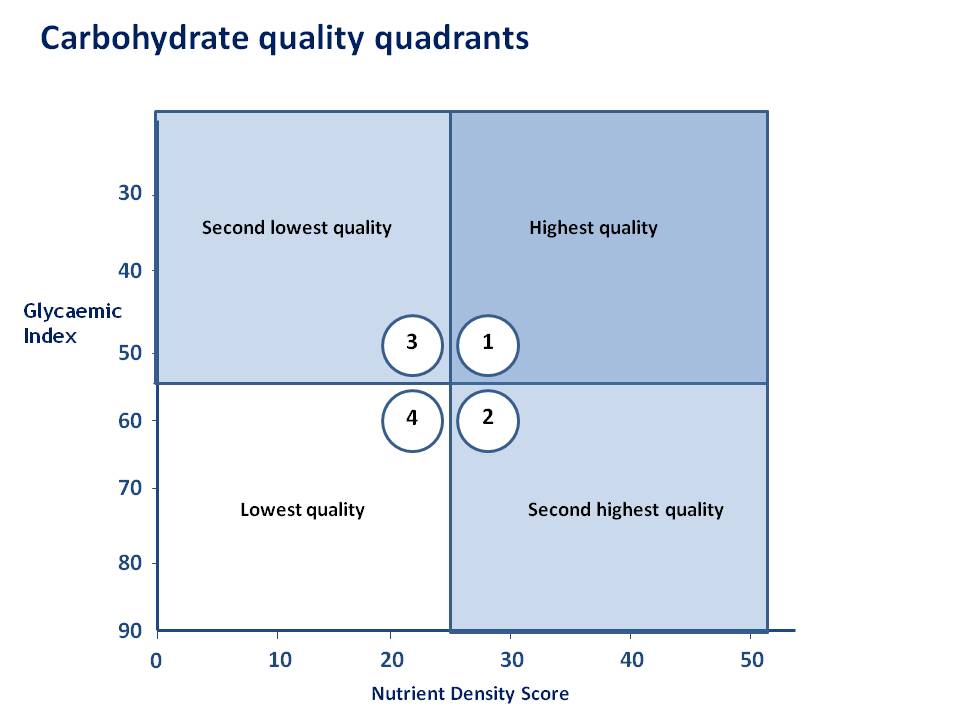
All results were plotted on the grid that appears in Figure 1, which is broken up into four carbohydrate quality quadrants. Quadrant 1 (high nutrient density, low GI) was considered to be the highest quality quadrant. Quadrant 4 (low nutrient density, high GI) was the lowest quality quadrant. To distinguish between the two intermediate quadrants nutrient density was prioritised over GI.
Figure 1:
The model showed considerable capacity to distinguish between groups of carbohydrate-rich foods. Of particular interest was whether the model was consistent with the dietary advice frequently offered in relation to these food groups. When legumes were run through the model they clustered in Quadrant 1– the highest quality quadrant, which was certainly consistent with the advice in most dietary guidelines (Figure 2).
Figure 2
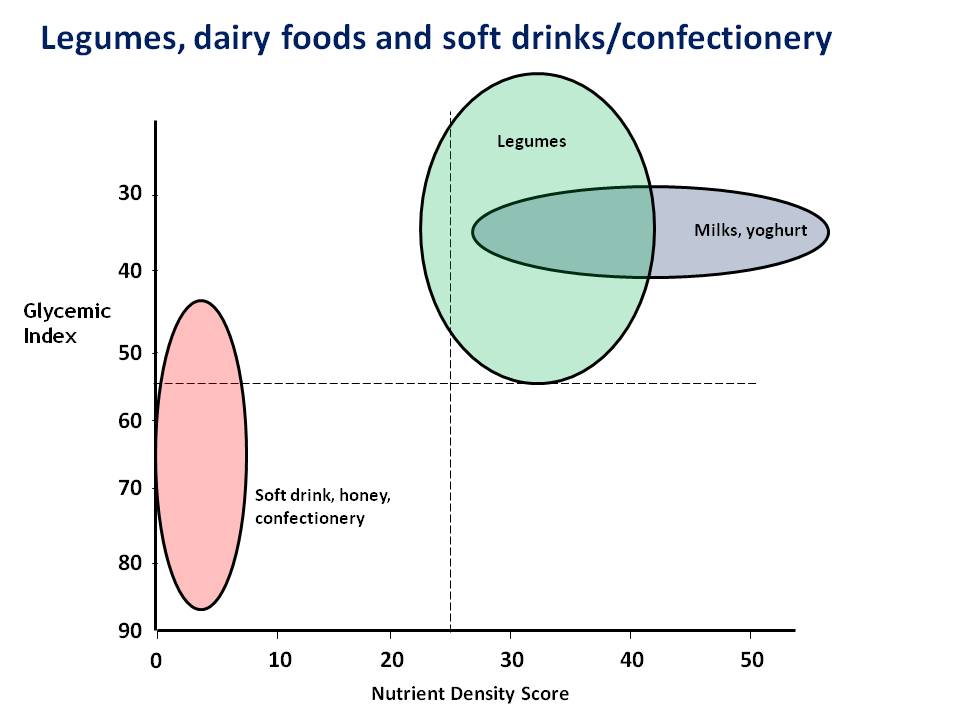
Milks and yoghurts appeared in the top quality quadrant too. The nutrient density of these dairy foods varied considerably due to the ‘nutrient dilution’ effect of the fat and sugar in some of these foods, but they all still appeared in Quadrant 1. In contrast, soft drinks, confectionery, honey and jam appeared in the lowest quality quadrant. Again, this was very consistent with mainstream dietary advice. So far, so good.
Fruits – a surprise
The model highlighted a few issues that might surprise some nutritionists. Firstly, fruits were not positioned as a tight group in one particular quadrant but were widely dispersed, mainly across Quadrants 1 and 3. In other words, the GI of fruits was typically low but nutrient density varied widely. Although fruits are often described as being nutrient-rich foods, some fruits such as apples, pears and grapes are actually quite nutrient-poor. The nutrient density of apple juice was similar to that of orange cordial. So fruits vary widely in their ability to provide the distinctive nutrients that this group of foods has to offer, though the generally low GIs are a plus.
Cereals – a conundrum
The cereal foods were also widely dispersed, being spread over all four quadrants but they were more concentrated in Quadrants 2 and 4, highlighting major differences in nutrient density. To make sense of the cereal foods I have divided them up into four groups (Figure 3):
• Biscuits, cakes, pastries
• Refined cereal foods (not enriched) – white rice, couscous, polenta, semolina
• Wholegrains (not enriched)
• Enriched cereals foods – breads and breakfast cereals
Figure 3
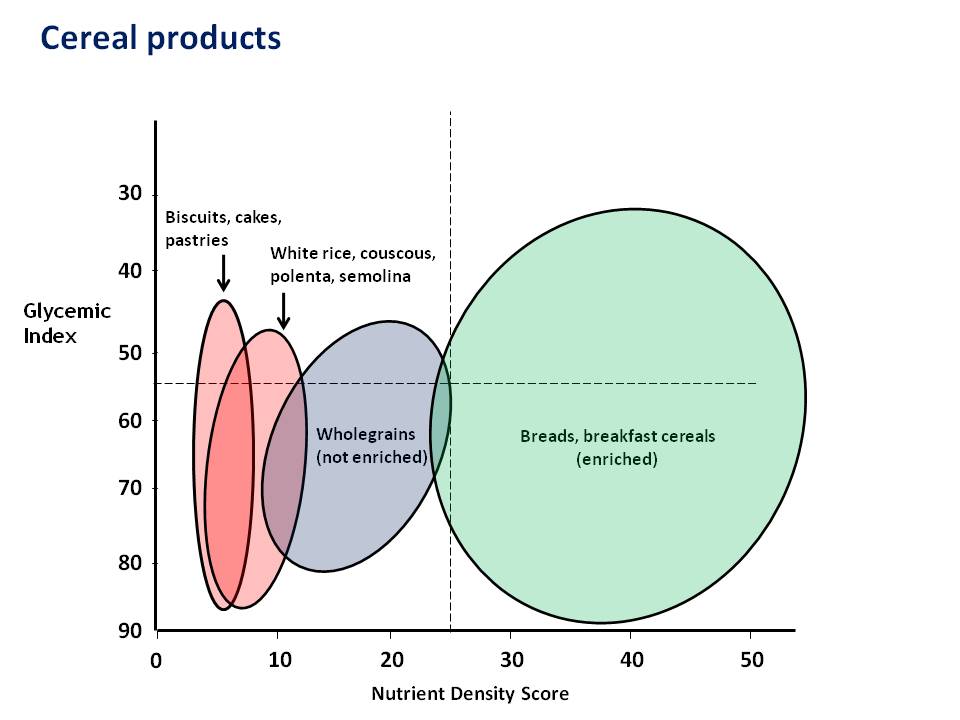
The model placed biscuits, cakes and pastries exactly where you would expect to find them – clustered in Quadrant 4, the lowest quality quadrant. This is consistent with traditional healthy eating advice to limit intake of these foods. But look where the model placed white rice, couscous, polenta, semolina – in virtually the same place. [Actually, the biscuits, cakes and pastries appear marginally to the left, their sugar and fat content resulting in a little ‘nutrient dilution’. However, refined cereal foods are so low in nutrients to start with that this effect is minimal.]
Until recently, white rice, couscous, polenta and semolina would have been preferred to biscuits, cakes and pastries on the basis of the latter foods’ higher saturated fat content. However, if high GI carbohydrate confers equal (or greater) risk for heart disease than saturated fat, this rationale no longer holds.
The next surprise was the relatively low nutrient density of non-enriched wholegrain foods. They were certainly more nutrient-rich than the refined cereals, notably the wholegrain wheat and oat products, but brown rice was positioned deep in the lowest quality quadrant. Wholegrains are frequently described as being nutrient-dense, but this is simply not the case.
The breads and breakfast cereals mostly fell in Quadrant 2, their nutrient enrichment predictably resulting in higher nutrient densities. The sugar content and the wholegrain status of breakfast cereals were unrelated to nutrient density as this was determined by nutrient enrichment.
What cereal foods should be recommended?
The Dietary Guidelines for Americans (2010) recommended that wholegrain and enriched cereals be included in healthy diets. The logic is clear – the wholegrains provide the fibre in under-supply in the American diet and the enriched cereals provide micronutrients. These recommendations are certainly consistent with our new model.
There is no dispute that biscuits, cakes and pastries should be limited – these foods carry plenty of calories but are nutrient-poor and many have high GIs. In nutritional terms, they have no redeeming features and are logical targets for reduction in healthy diets. However, all of these comments can equally be applied to white rice, couscous, polenta and semolina. Why do Australian nutrition authorities continue to recommend these foods in healthy diets? Doesn’t make sense.
What are your thoughts? How much cereal food should people eat? What type? And why?

Bill, seems to me you have under-played the role of fibre in the model, unless you see GI as a surrogate, which is not always the case. Diminishing the value of high-fibre wholegrains compared to enriched (and usually low-fibre) breakfast cereals seems an anomaly as well, and not a fair comparison for quadrant allocation.
Hi Paul
Fibre was included as one of the six nutrients for determining the nutrient density scores for legumes, grains, fruits and starchy vegetables, so it is built into the model. We thought long and hard about whether we should weight fibre higher than other nutrients. But why would you weight fibre higher than, say, thiamin, especially in a carbohydrate-constrained diet? Also, the Nutrient Reference Value for fibre is an Adequate Intake i.e. the precision about the requirement is lacking relative to thiamin, which is governed by RDI/EARs. So we thought we had the balance right.
In my conclusion I recommended wholegrains for fibre but the model demonstrates that they are not a great source of micronutrients (except for thiamin). If you want both fibre and ample micronutrients from the cereal foods group you really need a mix of foods. I think the Americans got this right recommending wholegrains and enriched cereals but our draft Dietary Guidelines’ recommendation for ‘mostly wholegrains’ misses the mark. Their dietary modelling was done using fortified wholegrain foods which drove the nutrient density of these cereal foods higher. Regards, Bill
Where does pasta fall?
Quadrant 3 – fairly low nutrient density but GI OK.
“Until recently, white rice, couscous, polenta and semolina would have been preferred to biscuits, cakes and pastries on the basis of the latter foods’ higher saturated fat content. However, if high GI carbohydrate confers equal (or greater) risk for heart disease than saturated fat, this rationale no longer holds.”
In regards to this comment… I find it somewhat disconcerting. Shouldn’t white rice, polenta and semolina still be preferred to biscuits, cakes and pastries? I know I would still recommend rice over cakes if they were the only 2 choices. Yes they are all high GI, but surely high GI PLUS high levels of saturated fats make the biscuits,cakes and pastries an unhealthier and poorer choice. I think your model is very useful and a worthwhile tool, but I also think we need to be careful the research coming out on carbohydrates and heart disease does not create a complete swing in which we place all blame on carbohydrates and forget that saturated fats are still a problematic nutrient.
Look forward to your comment.
Hello Leigh
The latest data is difficult to digest for all of us who were trained to think that carbohydrate is good and saturated fat is bad. However the latest evidence does tell us that the risks for coronary heart disease associated with saturated fat and carbohydrate are the same. So it follows that if you take carbohydrate (rice) and exchange half the calories for saturated fat (resulting in cake), there is no detriment or benefit. This isn’t saying that cake is better than we thought; it’s that rice is worse.
It is particularly challenging when you look at the evidence suggesting that high GI carbohydrate may actually confer greater coronary risk than saturated fat (Jakobsen MU et al. Intake of carbohydrates compared with intake of saturated fatty acids and risk of myocardial infarction: importance of the glycemic index. Am J Clin Nutr. 2010 Jun;91(6):1764-8.)
I agree entirely that saturated fat is a problematic nutrient. However, our advice needs to be that saturated fat in the diet should be replaced by unsaturated fats, not carbohydrate. As a consequence, healthy diets should be moderate in fat, not low in fat. Regards, Bill
to further add to the issue!
Could toasted muesli and soy beans (sources of polyunsaturated fat) be pushed up the nutrient density scale. As in a polyunsaturated fat replacing some of the carbohydrate in the food.
Hi Paul. As this was a model for carbohydrate-rich foods, there was effectively a macronutrient filter. So we excluded all macronutrients, including the essential fatty acids, from the nutrient density score.
This is a small bias against foods like muesli and soy beans that contain ‘good’ fats. And there is a small bias in favour of fat-containing dairy products which aren’t penalised for their saturated fat content per se. These are the exceptions rather than the rule, however. For me, the interesting part was where the various food groups were placed. Regards, Bill
Thanks for raising such an important issue – your presentation has certainly generated a great deal of discussion amongst dietitians. Cardiologist in Australia have been raising the issue of low CHO intake for heart health for some time in conflict with established nutritional advice. I have come across quite a number of clients who are trying to avoid breads and cereals, rice, pasta and potato on medical advice. We haven’t had a clear way of working out “healthy carbs” versus “unhealthy carbs” like we have with “healthy fats” and “unhealthy fats” so the advice is often coloured with opinion rather than using objective ranking. I would like to know what the rationale was for weighting nutrient density over low GI in order to rank quadrant 2 and 3? Kind regards, Megan
Thanks for your comments Megan. My response to the latest data is to recommend moderation i.e. not low fat; moderate fat. Not high carb; moderate carb. And to focus more on the quality of fat and carbohydrate. But as you point out the concept of carbohydrate quality is undeveloped, which is why we did the work.
Regarding the ranking of Quadrants 2 and 3, one option was to rank them equally. In the end it was difficult for these nutritionists to favour nutrient-poor foods over nutrient-rich foods, irrespective of the GI.
To my mind the key is which foods ended up in Quadrant 4, the lowest quality quadrant. If we are to recommend more moderate carbohydrate intakes in future, this is where I would be looking to make some cuts. Regards, Bill
Thank you for this perspective of foods. Instead of using GI why not Glycaemic Load. It would make a better sort on the fruits and some of the vegies such as pumpkin and carrot which on one of the slides makes these indistinguishable from say potatoes.
Hi Deidre. Our reviewers asked exactly the same question. The reason for choosing GI rather than GL is as follows. Of course, GL considers both the GI and the amount of carbohydrate. All of the foods in the model are carbohydrate-rich foods and calculations for each food were based on the same amount of energy (600kJ). So the amounts of carbohydrate in each comparison were similar. In other words, amount of carbohydrate was almost a constant. In this context GI becomes the discriminating factor. Regards, Bill
Bill and Manny I am interested to see your graph for starchy vegetables, perhaps potato will need one all on its own. I am sure the variation in the fat and water content between the humble steamed potato with skin v. deep fried skinless chip would change both GI and nutrient density values. The potato is such a significant factor in the diet of westernised communities I am interested in your opinion as a comparable ‘carbohydrate’ food to the cereals mentioned. It would be interesting to see it compared with cassava, taro as an alternative used by Islander and African communities in Australia. I also understand that the Australian Dietary Guidelines modelling did not put potato with vegetables, and I have not read the fine print to know what the other ‘starchy veg’ were included?
Hello Fiona. Your instincts are right. We put boiled potato, French fries and potato crisps through the model. The boiled potato appeared in Quadrant 2 (second highest) and the French fries and potato crisps ended up in Quadrant 4 (lowest), so there was considerable nutrient dilution by fat and presumably some loss of nutrients by the processing. GIs for French fries and potato crisps were lower than for boiled potato but not enough to take these foods out of Quadrant 4.
Potato performed better than refined cereal foods and unenriched wholegrains, due to potato’s higher nutrient density. Potato appeared in the same quadrant as enriched cereal foods.
We were limited in the range of foods we could put through the model by the availability of GI data, so cassava and taro didn’t get a run. Not sure if these data are available now.
Every aspect of the Dietary Guidelines process perplexes me.
Regards, Bill
I love this Bill! I think its spot on and goes in line with how I educate others on carbs. Thank you for sharing it in a scientific and graphical way! I am curious, what were the 6 nutrients that were assessed? Fibre and..? Were omega 6′s taken into consideration or is this still on the edge given the mixed reviews about them and their effects on health?
Hi Kara. We chose the six distinguishing nutrients of each food group. So our nutrient density score measures the potential of a food to deliver the nutrients characteristic of its food group.
Legumes Iron, fibre, folate, magnesium, vitamin B6, potassium
Bread, cereal products Thiamin, riboflavin, niacin, iron, fibre, folate
Fruits Vitamin C, folate, fibre, vitamin B6, potassium, vitamin E
Starchy vegetables Vitamin C, fibre, vitamin B6, potassium, magnesium, thiamin
Dairy foods Calcium, vitamin B12, riboflavin, vitamin A, potassium, zinc
Confectionery, condiments Six major micronutrients in each food
If you assess nutrient density within food groups you only need to consider a relatively small number of nutrients (six is ample). We excluded macronutrients, so no omega 6 or omega 3. Regards, Bill
Thanks Bill for explaining that. One more question. Would it not be useful to look one step deeper at something like antioxidant levels? I would think that some of the benefits of consuming whole-grains over fortified products are in the non nutritive beneficial properties such as these. Overall I think the fusion of glycemic index and nutrient density is a fantastic approach and I would love to see this pushed into a more mainstream way of thinking for all consumers and health professionals out there! Again, thank you for sharing.
Hi Kara. You have raised an important issue. This is how we dealt with it in the Discussion of our paper.
“… it should be recognised that different carbohydrate-rich foods may vary in the risk they confer relative to saturated fat and all of this variation may not be captured by GI. For example, the potential benefits of phytonutrients in legumes, cereals, fruits and vegetables have not been considered as reliance on only those nutrients with accepted nutritional roles was thought to be the most robust approach.”
In developing our nutrient density score we followed the lead of Drewnowski who argues that only nutrients with Nutrient Reference Values should be considered. We carried that approach through to other aspects of the model.
Can I add that I am very sceptical about the benefits of dietary antioxidants, with the exceptions of vitamins C and E. The role of antioxidants in the prevention of heart disease and cancer has been overstated. Polyphenols may well turn out to be protective and they are antioxidants but the mechanism of their protection does not appear to be anti-oxidation. Regards, Bill
I’m glad you brought up polyphenols. Polyphenols of fruits and berries may be effective in reducing (post-prandial) inflammation, and glycemic & insulinemic responses, see for example Törrönen et al. 2012 (AJCN) or the recent apple vs plum RCT by Chai S et al. 2012 and orange juice plus standard meal studies. Polyphenols also increase NO production to some extent, and thereby augment arteries.
Hello Reijo. For our model we followed the recommendations of Drewnowski closely and one of these was to only use nutrients with accepted nutritional roles i.e. nutrients that had Nutrient Reference Values. So, fibre was in but polyphenols were out.
I have to admit that I am in two minds about polyphenols. On the one hand there are the beneficial effects that you mention but on the other hand polyphenols are also known to adversely affect mineral absorption, especially iron absorption. With up to a third of young women in this country with some degree of iron deficiency I’m a bit reticent to recommend lots of polyphenols for all. What are your thoughts on this? Regards, Bill
I’m not really sure how you can compare whole grains with breakfast cereal. The main reason breakfast cereal is included in this comparison is due to the high carbs, which are a result of the ingredients… which are largely rice and whole grains. So obviously if you mix enough “good stuff” together you’ll get a superior food with a higher nutrient density. People are generally eating whole grains for a reason – the quality fiber, and the lack of other “stuff” that goes into enriched products. So while these products may contain a ton of nutrients, that (to me) does not necessarily mean better. A lot of people prefer to get specific nutrients from specific places.
I guess my main point is that I don’t think a product should be compared on any stage with the ingredients that went into it.
You are right to argue that wholegrains mainly provide fibre (and thiamin). However, if everyone just ate un-enriched wholegrains the population’s intake of a range of B vitamins and iron would be lowered considerably. Shifting a population’s intake of nutrients lower increases the probability that nutrient deficiencies will occur.
Nutrient enrichment is a fundamental public health nutrition strategy. Its purpose is to ensure that the least educated person, in the lowest socio-economic group, with the poorest diet has a good chance of avoiding a vitamin deficiency disease. And it works well. Regards, Bill
Over all this model appears to be quite good but one food that appears to be poorly rated was rolled oats which sits not too far away from milk chocolate and potato chip. If we were to accept this then there would not be too much difference in having a bowl of porridge or pack of small fries for breakfast. Coco pops comes out with a much better position due to the fortification. what is your take on this, are RO really this bad?
Hello Jeremy. The idea of this model was to use objective criteria to categorise the nutritional quality of carbohydrate-rich foods. This means one has to park preconceived ideas about what’s healthy and what’s not at the outset.
For me, one of the surprises to come out of this exercise was the poor showing of unfortified cereal foods. Over the last decade or so our message about such foods has been to ‘eat plenty’. I think we really need to re-examine this. In fact, with many unfortified cereal foods we should ask why these foods should not be restricted.
The model puts rolled oats and coco pops in the intermediate quality categories – rolled oats has low nutrient density but low GI as well; coco pops has more nutrients but a higher GI. I would not read this as advice to avoid eating rolled oats.
If I were recommending lower carbohydrate intakes (and I do) I would target those foods in carbohydrate quadrant 4 – the lowest quality quadrant. They really have no redeeming features. LOTS of our dietary carbohydrate comes from foods in this sector.
Regards, Bill
“With up to a third of young women in this country with some degree of iron deficiency I’m a bit reticent to recommend lots of polyphenols for all. What are your thoughts on this? Regards, Bill”
I was not aware of the effect of polyphenols on iron absorption. It is a valid point even if I’m not sure of the magntude of the effect. Berries and fruits, major sources of polyphenols, also are high in vitamin C. Vitamin C increases the absorption of iron. Are you aware of clinical trials on blue berries, cranberries, blackcurrants, strawberries, oranges or fruits that had shown clear negative effect on iron absorption? Perhaps avoiding too much green tea and coffee would advisable among younger women, as they are almost devoid of vitamin C? Here in Finland, coffee is the biggest source of polyphenols in diet.
Iron status among Finnish young women is also rather low. So this is a real problem and dietary instructions should be adjusted on individual basis. The situation is different with males.
I think the same problem of decreased iron absorption relates also to dairy products (calcium) and whole grains (phytates). I would not generally advise my patients to use less of them because of their affect negatively iron absorption. In males, decreased iron absorption may even be of benefit, as Harvard and other prospective cohorts have suggested (red & proccessed meat studies). What do you think?
Reijo, if polyphenols prove to be beneficial maybe the best way of increasing intake is through beverages (tea/coffee) consumed between meals.
Agree there is an issue with phytates in wholegrains (and nuts) in relation to iron absorption. And this is one reason that I am cautious with cereal advice to eat ‘mostly wholegrains’. For some people this may have adverse consequences. Moderation, even of wholegrain intake, is a sound nutrition principle.
Regards, Bill
Hi Bill,
I am just reblogging your findings to get your word out a bit more! I am looking at your powerpoint presentation from the IG seminar. White rice is right at the bottom with a GI of 80. Just wondering though, how about long grain rice like basmati which are moderate in GI (= 57)? Considering how rice is such a staple food in Asian cultures and people are used to having so much of it on their plate, what are your suggestions for replacing this in a culturally sensitive way. Which varieties of rice, if any, were considered good carbohydrate by the model? Thanks in advance!
Hello Nazzah
When Frank Hu from Harvard was in Sydney earlier in the year he presented some of their work about how it might be possible to encourage Asian populations to eat less white rice. In one study they looked at the acceptability of brown rice and the results were not that good. There were cultural barriers – brown rice was considered to be inferior. Changing rice type, as you mention, could be a way forward.
Also, as Asian populations become wealthier it would be expected that the people will eat more protein and fat, and less white rice. In nutritional terms, this may be beneficial – glycaemic load falling. But it will be accompanied by increased calorie intake so it may be a case of one step forward and one step back.
Regards, Bill
PS. Regarding rice used in the model, I would have to check. One limitation for us was the availability of both good nutritional data and good GI data.
Thanks Bill. In regards to the weighting you used in the model, couldn’t you weight fibre that is beta glucan a bit more so that foods like oats would move higher up where they are more likely to belong (away from the coco pops)? Otherwise, I strongly agree with the gist of promoting quadrant 1 foods and demoting quadrant 4 foods, to cut down unnecessary carb intake. Cheers!
Otherwise, I strongly agree with the gist of promoting quadrant 1 foods and demoting quadrant 4 foods, to cut down unnecessary carb intake. Cheers!
I am an elderly layperson, Bill, and I would like to know if there is any evidence that Asian populations (whose rice intake per capita would be vastly higher than non-Asians) have experienced relatively degraded health as a result of eating Quadrant 4 rice.
Hello Frank
In March 2012, the British Medical Journal published an analysis of studies that had investigated associations between the consumption of white rice and the risk for type 2 diabetes. Here are the study’s conclusions:
“In summary, this meta-analysis suggests that higher white rice intake is associated with a significantly elevated risk of type 2 diabetes, especially among Asian populations. The recent transition in nutrition characterised by dramatically decreased physical activity levels and much improved security and variety of food has led to increased prevalence of obesity and insulin resistance in Asian countries.39 Although rice has been a staple food in Asian populations for thousands of years, this transition may render Asian populations more susceptible to the adverse effects of high intakes of white rice, as well as other sources of refined carbohydrates such as pastries, white bread, and sugar sweetened beverages. In addition, the dose-response relations indicate that even for Western populations with typically low intake levels, relatively high white rice consumption may still modestly increase risk of diabetes.”
Regards, Bill