One of the more commercially driven myths circulating at present is the idea that somehow saturated fat is better for health than carbohydrate. Virtually all the low carb advocates push this argument, but why would they do that?
The changing science
The science relating to how much of what we should eat for good health has certainly evolved in recent decades, but it’s not a simple story.
• In the early 1980s, most health authorities recommended that saturated fat in the diet should be limited to lower heart disease risk.
• At that time trans fats were thought to be neutral but by the 1990s they were considered be as bad as saturated fats. And by the 2000s trans fats were thought to be worse than saturated fat.
• Three decades ago carbohydrate was thought to be the ideal replacement for saturated fat, which led to widespread support for low fat diets. But by the late 2000s scientific support for low fat diets had dropped away.
• Although the early science indicated that unsaturated fats may be the best option to replace saturated fat in the diet somehow they were less preferred to carbohydrate. Their time has now come.
The Willett Model
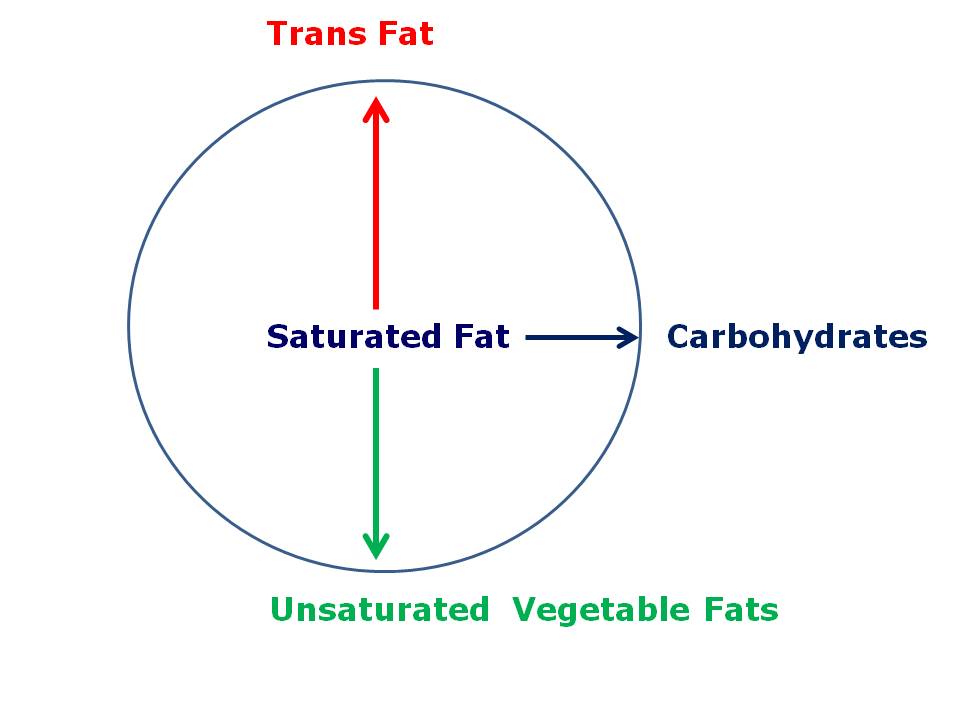
Harvard nutrition guru Professor Walter Willett has developed a simple model for explaining the current state of the science. His model puts saturated fat at the centre of our attention and then shows how heart disease risk is affected when other nutrients replace it in the diet.
Key points to note are:
If trans fats replace saturated fats in the diet, heart disease risk goes up. So trans fats should be minimised in the diet, which has been successfully achieved in Australia.
If unsaturated fats replace saturated fat, heart disease risk goes down. The resulting Mediterranean-type diet is moderate in total fat but enriched in unsaturated fats. This is now the preferred foundation for a heart-healthy diet.
Which brings us to the third point: there is no advantage in replacing saturated fat with carbohydrate, or vice versa. Heart disease risk is unchanged. The big lesson for nutritionists from this was to stop advocating low fat diets for heart disease prevention. The other lesson – for the general public in particular – is to ignore all the rhubarb from low carbohydrate advocates who argue that we should all eat more saturated fat, in general, and more coconut oil in particular. It has no basis in science.
Dubious motives
The motives of the saturated fat enthusiasts are particularly dubious. Not content with pushing the myth that saturated fat is better for health than carbohydrates they further muddy the waters by demonising ‘seed oils’, which is code for unsaturated fats. So we are asked to believe that carbohydrate and unsaturated fats are both evil and therefore the only safe thing for us to eat is saturated fat. Claptrap of the highest order.
Needless to say, all of the world’s leading nutrition authorities do not support these arguments.
If your suspicions were not already fully aroused, ask yourself why these dietary myths are pushed by non-nutritionists via social media. Hmmm, you don’t think it could be a thinly-veiled marketing campaign for coconut oil, do you?

Wow!! Cool conspiracy theory Bill! The coconut oil conspiracy! As a successful low-carber I am seriously amused! My doc put me on a low carb diet to resolve insulin issues and it worked! And I continue to use a wide variety of fats and oils based on their chemical stability and benefits.
Except the argument wasn’t about insulin instability, for which a low carb diet is ideal (depending on the nature of the impaired insulin response), the argument is that increased saturated fat has a scientifically based association with increased cardiovascular disease risk.
Hi Bill,
Have been doing some reading around Dean Ornish and his well documented improved in coronary revascularisation. Would love to hear your thoughts.
…as well as the meat/dairy/egg industries, at least in the United States. Take a gander at the full literature for the Beef Checkoff program. It includes results-predetermined anti-carb studies. (Volek study is listed as “achieved”)
The latest study by the Harvard group contains a graph of plasma linoleic acid v.s. mortality. The graph is a hump-shaped snapshot of intakes of linoleic acid ranging above and below average intake in the United States. Highest mortality is for intakes approximating average LA consumption in the United States. ” The association between dietary circulating LA concentration was nonlinear. Circulating LA showed the greatest dose-response association with intake of LA up to ~8% of total daily energy; with relatively smaller increases at intakes>8%.” At intakes of LA greater than 8% one would expect carbohydrate and saturated fat consumption to taper off because that was a design feature of the study. It is unlikely any significant number of subjects consumed less than 5 % LA so the only data we have for lower intakes of LA is derived from Lyon Diet Heart Study. Among other interventions, the study arm reduced intake of LA to 3.5%. The result was a 70% reduction in morbidity and mortality. The benefit was so significant that the 5 year study was terminated at 27 months. The Lyon study, being the only long-term study of its kind, can only hint at what would happen if linoleic acid intake were lowered to historic intakes amounting to 2% of calories or less.
Experimental evidence suggests LA and fructose together are disastrous. “The incidence of obesity in the U.S. has increased from 15% to 35% in the last 40 years and is expected to rise to 42% by 2030. Paralleling this increase in obesity are a number of dietary changes, most pronounced of which is a >1000 fold increase in consumption of soybean oil from 0.01 to11.6 kg/yr/capita from 1909-1999: soybean oil consists of 50-60% linoleic acid (LA), so the energy intake from LA has increased from 2% to >7%/day.” http://press.endocrine.org/doi/abs/10.1210/endo-meetings.2013.OABA.9.SAT-708
Hello David. Most of the Harvard studies are supportive of linoleic acid. What Harvard study are you referring to? Regards, Bill
http://circ.ahajournals.org/content/early/2014/08/14/CIRCULATIONAHA.114.011590.full.pdf+html
Check out Figure 2 on page 27.
Are we thinking of the same Lyon Heart Study? AFAIK the study was halted because the polyunsaturated fat intervention group did so well at the time that the researchers felt it was unethical to continue to let the control group suffer the consequences of their usual diet.
AFAIK the Lyon study control group had higher linoleic aciid and overall PUFA intake.
The intervention group had lower LA, higher omega 3 intake.
The cholesterol levels of both groups were not significantly different, but the CHD mortality was.
The Farvid et al. 2014 meta-analysis, the one in which linoleic acid substitution looks good for heart disease events and mortality, does actually support the idea that saturated fat is better than carbohydrate.
It says that 5 percent energy intake from LA replacing the same amount of energy from carbohydrates was associated with a 13% reduction in CHD mortality. This is exactly the same as the reduction in CHD mortality associated with 5% energy intake from LA replacing the same amount of energy from SFA.
So for CHD mortality, CHO and SFA are exactly equal (the CIs are identical too).
So let’s look at CHD events for the tie breaker:
The risk estimate for substituting 5% energy intake from LA for carbohydrates was 0.90 (95% CI, 0.85-0.94) with a fixed-effect model and 0.89 (95% CI, 0.80-0.98) with a random-effects model.
The risk estimate for substituting 5% energy intake from LA for SFAs was 0.91 (95% CI, 0.87-0.96) with a fixed-effect model and 0.90 (95% CI, 0.80-1.01) with a random-effects model.[1]
For CHD events, saturated fat is better than carbohydrate. In the random-effects model, replacing SFA with LA didn’t even pass significance.
(consistent with the properly randomised and controlled RCTs of fat substitution, which have an RR of 1.00 in meta-analysis) [2]
Now, this isn’t refined carbohydrate – it’s mixed carbohydrate that includes carbohydrate from vegetables, fruit, and wholegrains. If you think those carbs would look better, in that case refined carbs would look worse.
Further, carbohydrate is a macronutrient, saturated fat is a macronutrient subtype.
Every fat that supplies saturated fat supplies some PUFA. Even coconut oil has a little bit. Which seems to make fat better than carbohydrate overall, but remember this is just epidemiology.
[1] Dietary Linoleic Acid and Risk of Coronary Heart Disease: A Systematic
Review and Meta-Analysis of Prospective Cohort Studies. Farvid MS, Ding M, Pan A, et al.; 2014.
DOI: 10.1161/CIRCULATIONAHA.114.010236
[2] Emphasising ‘Randomised’ and ‘Controlled’ in a Meta-Analysis of Randomised Controlled Trials regarding Saturated Fat and Coronary Heart Disease. Steve Hamley. Blog Post meta-analysis using Review Manager V.5.1 software (RevMan), provided by the Cochrane Collaboration. Tuesday, March 31, 2015.
http://www.stevenhamley.com.au/2015/03/emphasising-randomised-and-controlled.html
“For CHD events, saturated fat is better than carbohydrate.”
Oh yes, so very much better indeed.
“Now, this isn’t refined carbohydrate – it’s mixed carbohydrate that includes carbohydrate from vegetables, fruit, and wholegrains. If you think those carbs would look better, in that case refined carbs would look worse.”
… and since the study populations have been Westerners, it’s been MOSTLY refined carbs as that is – unfortunately – what we eat. In addition, bear in mind that the effects of safa intake have likely been attenuated by e.g. its intake from fermented dairy products (foods relatively rich in safa which have ingredients that tone down the effect of safa on lipid levels).
Hello Mie. Echoing my reply to George, I don’t yet understand how carbohydrates confer the coronary risk that they do. The current vogue is to blame sugar for everything though I suspect glycaemic index/load is important. If it is, we need to be careful about how we advise people on carbohydrate-rich foods. For example, wholemeal bread isn’t usually considered a refined carbohydrate yet it has a high GI.
Carbohydrate quality is a complex subject and am sure we will hear a lot more about it in the next decade, Regards, Bill
Hello George. Why do you think carbohydrate is (roughly) equivalent to saturated fat in relation to CHD mortality/events? Based on effects on LDL-C you would expect carbohydrate to be protective, so another mechanism(s) must be at play. What do you think it is? Regards, Bill
Bill, if I was to go with serum lipids, I would say that the effect of CHO is mediated through post-prandial triglycerides, with the depleted VLDL particles playing the role usually attributed to LDL.
We have a situation where the risk of diabetes is common and the effect of glycosis on blood vessels should also be considered. However, the difference between SFA and mixed CHO in Farvid et al. is slight, there is a similar relationship in Jakobsen et al., but there is no reason to read much into it. Generally any energy source that is not PUFA increases CHD to much the same extent if it is substituted for PUFA in this type of analysis.
Except perhaps if they measured fibre and protein, but these are as rare as PUFA, and the analyses may just be showing up the value of scarcity.
Certainly if wholefood carbs – carbs from fruit and veges, which Westerners do eat, and wholegrains, which they might depending how this is defined, are thought to be healthier than refined carbs, then isolating refined carbs in a substitution meta-analysis (which should be done some day soon) will surely show them to be more strongly associated with CHD than any fat type.
But how much of this effect will be due to diabetes, metabolic syndrome, insulin resistance, in other words, on the effect of carbohydrates in people who don’t tolerate them very well for medical reasons, and how much – if any – is intrinsic to sugar and starches, which seem to be healthy enough in some populations?
But what would be the message to send to the population, that SFAs are healthy? That would be wrong when you look at the whole picture. Clearly we’re still lacking strong and well-designed prospective cohort study to know the full effect of SFAs on CHD risk. Making matters more complicated, different SFAs might have different effect, and comparing it to another nutrients does not have the same impact. We know that less SFAS, more PUFAs decrease risk. The effect of carbs and MUFAs are less clear as of now.
But, let’s look at the full picture.
SFAs might impairs IS. Not yet clear, studies are conflicting.
SFAs looks inflammatory, primilarly but not exclusively through an impact on the microbiome
Diets high in saturated fat increase intestinal inflammation associated with IBD via alterations in the microbiota
Influence of dietary fat on intestinal microbes, inflammation, barrier function and metabolic outcomes
A saturated fatty acid–rich diet induces an obesity-linked proinflammatory gene expression profile in adipose tissue of subjects at risk of metabolic syndrome
Differential Effects of Cream, Glucose, and Orange Juice on Inflammation, Endotoxin, and the Expression of Toll-Like Receptor-4 and Suppressor of Cytokine Signaling-3
Consumption of Saturated Fat Impairs the Anti-Inflammatory Properties of High-Density Lipoproteins and Endothelial Function
In mice, a high SFAs, LC diet increases mortality
High saturated fat and low carbohydrate diet decreases lifespan independent of body weight in mice
SFAs might impairs endothelial function, althought studies are conflicting
SFAs do not impair endothelial function and arterial stiffness
Flow-Mediated Dilatation Is Impaired by a High–Saturated Fat Diet but Not by a High-Carbohydrate Diet
SFAs is most likely to results in abdominal fat accumulation compared to PUFAs
Overfeeding Polyunsaturated and Saturated Fat Causes Distinct Effects on Liver and Visceral Fat Accumulation in Humans.
SFAs are obegenics
Saturated fat stimulates obesity and hepatic steatosis and affects gut microbiota composition by an enhanced overflow of dietary fat to the distal intestine
Whole body oxidation of dietary fatty acids : implications for energy utilization
Differential oxidation of individual dietary fatty acids in humans
Increasing dietary palmitic acid decreases fat oxidation and daily energy expenditure
And I mean this is only the tips of the iceberg. This is far from looking healthy to me and anyone in for the science should at least still be very cautious on how they interpret the evidence and what kind of recommendations comes out of it. It really does not look to me as if increasing SFAs is a good idea at all.
Bill how familiar are you with Mozzaffarian’s resent research into SFA’s and are you able to sum them up for me? He is often quoted by advocates of high fat diets and when I go to read his studies I get confused (I don’t have the background ). Is he suggesting we re think the role of SFA in the diet or is he being quoted out of context.
Reply no longer needed Evelyn at Carb-Sane Asylum has been following him and blogged on him.
Hi Bill, I just wondered what are your thoughts on this recent paper:
The association of substituting carbohydrates with total fat and different types of fatty acids with mortality and weight change among diabetes patients.
Clin Nutr. 2015 Aug 28. pii: S0261-5614(15)00224-1. doi: 10.1016/j.clnu.2015.08.003.
http://vernerwheelock.com/?p=191m
Margarine is yesterday’s hero