New research has strengthened the case that the glycaemic index of carbohydrate-rich foods affects the risk for cardiovascular disease and is a useful tool in weight management. But Australian health authorities are in denial, refusing to even look at the data.
Four decades ago nutritionists were taught that complex carbohydrate (starch) was desirable as it was slowly digested and absorbed, which led to a gradual rise in blood glucose and this was considered to be a good thing. In contrast, simple sugars were thought to be rapidly broken down and absorbed, giving a high blood glucose response. Although logical enough, it wasn’t true.
When the blood glucose-raising effects of various foods were actually measured it was found that some starchy foods, such as potato and rice, produced very rapid increases in blood glucose to high levels – higher than that of table sugar. Use of the terms simple sugars and complex carbohydrate is now discouraged by the World Health Organization.
What is GI and glycaemic load?
Differences in the blood glucose-raising effects of carbohydrate-rich foods are now described using the glycaemic index (GI). The GI of pure glucose is 100 and other foods are compared against it. The GIs of starchy foods vary widely from about 100 for potato down to about 20 for soybeans. The low GI of soybeans and other legumes is due to slow digestion of the starch in these fibre-rich foods, resulting in a low, flat blood glucose response.
Some of the studies discussed below use the term glycaemic load, which incorporates both the GI and the total amount of carbohydrate consumed. A high glycaemic load results from a high intake of high GI foods. Therefore glycaemic load can be lowered by eating less carbohydrate, eating lower GI foods, or both.

Image: source
GI and health: the Harvard studies
Possible adverse health effects of high GI foods and high glycaemic load were identified in the Nurses’ Health Study and the Health Professionals Follow-Up Study conducted by the Harvard School of Public Health in the United States. In 1997, GI and glycaemic load were found to be associated with increased risk for type 2 diabetes in women and men. A few years later glycaemic load was found to be associated with increased risk for coronary heart disease and then stroke in women. In these studies the associations were strongest among women who were overweight. Higher glycaemic load was also associated with higher levels of the inflammatory marker CRP in the bloodstream, consistent with higher risk for cardiovascular disease.
How does GI work?
David Ludwig discussed plausible mechanisms that would explain adverse effects of high GI foods and high glycaemic load in an excellent paper in the Journal of the American Medical Association. In relation to the risk for coronary heart disease Ludwig suggests that part of the problem may be oxidative stress caused by high blood glucose levels after meals. This would activate inflammation and perhaps explain the associations between glycaemic load and inflammatory markers.
Ludwig considers insulin to be central to the risk posed by high glycaemic load. He suggests that the regular consumption of high glycaemic index meals results in a cycle of high insulin levels and insulin resistance that increases the risk for diabetes and the metabolic syndrome, with its associated risk for cardiovascular disease. This may explain why glycaemic load appears to pose greater risk to those who are overweight and therefore more likely to be insulin resistant already.
Ludwig also argues that a high insulin level after a high GI meal leads increased hunger several hours afterwards, increasing the possibility that food intake will be in excess of calorie needs. If GI affects hunger and satiety it could be a useful tool in weight management.
GI and weight management: the Diogenes Study
The role of GI in the maintenance of weight loss was recently tested in a large, randomised controlled trial in Europe. In the Diogenes Study the subjects initially lost 8% of their body weight and were then placed on one of five weight maintenance diets, differing in protein content and the GI of the carbohydrate. Essentially, the diets differed in their glycaemic load as the higher protein content was achieved by lowering carbohydrate. There was no calorie restriction in this stage of the study and the subjects were expected to start to re-gain weight. The figure below shows the effects of the different diets on weight re-gain.
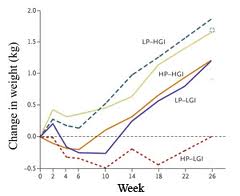
Image: source
The study found that both higher protein content and lower GI had beneficial effects on weight re-gain. The diet with the lowest glycaemic load – high protein and low GI – was associated with no weight re-gain at all after 26 weeks. And the diet with the highest glycaemic load – low protein and high GI – resulted in the greatest weight re-gain. As calories were not being restricted, it can be assumed that the different rates of weight re-gain were a consequence of differing hunger and satiety. Maybe David Ludwig was right.
Other recent findings
In a more recent paper from the Diogenes study, the lower GI diets were associated with lower levels of the inflammatory marker CRP, confirming the finding in the observational studies. This is in contrast to the lack of effect of wholegrains on CRP in an intervention study mentioned in last week’s blog.
A European cohort study recently confirmed that dietary carbohydrate was associated with the same risk for coronary heart disease as saturated fat. However, when the GI of the carbohydrate was considered, low GI carbohydrate was associated with less risk (non-significant) than saturated fat but high GI carbohydrate was associated with significantly higher risk than saturated fat.
GI and the Australian Dietary Guidelines
No doubt you will want to read how these new findings are interpreted and translated into dietary advice in the forthcoming Australian Dietary Guidelines, but you may be disappointed. For reasons known only to the powers-that-be, the role of GI in health was not the subject of a single systematic literature review in the development of the draft Dietary Guidelines recently circulated for consultation. How can national dietary guidelines purport to be based on the latest scientific evidence when significant parts of the literature are totally ignored?
Maybe this turning a blind eye to GI is driven by embarrassment. In recent decades the health authorities encouraged the general public to lower their intake of fat as part of a strategy to address the obesity epidemic. Example A of the last Australian Guide to Healthy Eating restricted both fats and major sources of protein, and encouraged intake of high GI carbohydrate-rich foods to fill the gap. This high glycaemic load prescription was similar to the worst performing diet in the Diogenes study.
The case that GI is relevant to health has strengthened in recent years and this parameter needs to be considered when the nutritional quality of carbohydrate-rich foods is assessed.
I’ll be overseas for a couple of weeks and will respond to your comments on my return.

I remain skeptical of the utility of the GI and its association with chronic disease. Most people consume carbohydrates in combination with protein and fat, which can dramatically change the GI of a food. Stanhope et al showed the calculation of the GI for mixed meals to be unreliable, overestimating the true GI by 22-50%…this was with small amounts of protein and fat in the meal. Fabricatore et al showed the GI to have some predictive value in terms of predicting some blood glucose metrics in overweight and obese people, but the predicting power was weak and the GI could only account for 10-18% of the variance. The individual data was all over the place in this study; some days with the highest glycemic diets scored the best on metrics of glycemia. In the Diogenes study, they only achieved a 4.7 point difference in GI. While much of the data on GI might be statistically significant, but I question the biological significance. I think GI is more of a proxy for overall diet quality (i.e., a diet rich in whole fruits and vegetables) , which is why you see associations with chronic disease.
Hi James. Long live scepticism! In relation to GI, I sat on the fence for 15 years – there just wasn’t enough evidence to convince me. But with the new studies I reviewed in my blog I think GI has to at least be considered. The evidence that GI is related to health is stronger than that for sugar and health. I can’t see how you can base dietary guidelines around sugar but not GI. It should be both or neither. Not sure about your idea about GI being a proxy for overall diet quality. Fruits generally have low GI; many wholegrains have high GI – there are many anomalies. That’s what makes carbohydrate quality such a challenging concept. Regards, Bill
I truly enjoyed reading it. Waiting for some more great stuff like this from you in the coming days.